Thoughts, Inspiration, And Stories
About Healthcare

Can you use boric acid on your period?
Overview Boric acid is totally safe to be used during your period in the form of a suppository. It’s not recommended or preferred in

Leukocytes in urine: Is it a sign of infection?
Overview High leukocytes in urine can indicate an infection such as a urinary tract infection or inflammatory medical condition, including kidney infection or stones.

Nausea after eating: Causes, Treatment, and Prevention
Overview Are you feeling nauseous, followed by a vomiting episode after you are done having your meal? Something is not up to the mark

How to relieve stomach pain and diarrhea?
Overview Stomach pain and diarrhea can be treated after identifying the right cause. Minor underlying conditions like allergic reactions, indigestion, or stomach flu go

How long to wait for sex after yeast infection treatment?
Overview A yeast infection, while common, can disrupt your daily life and intimate relationships. If you’ve recently been treated for a yeast infection, you

Body aches, chills and no fever? What could it be?
Overview Body aches and chills can be accompanied with or without a fever. Body aches can result from a multitude of causes, including inflammation

Can I take a decongestant while pregnant?
Overview Even a simple cold or allergy flare-up can feel overwhelming when you’re pregnant. You want relief, but the usual go-to medications suddenly come

Can allergies make you cough?
Overview If you’ve ever asked yourself, “Can allergies make you cough?” you’re not alone. Many people experience a persistent cough during allergy season and
Categories
- Allergy (12)
- Cancer (9)
- Cardiology (4)
- Dermatology (19)
- Endocrinology (1)
- ENT (25)
- format-2024 (9)
- Gastroenterology (20)
- Health Care (55)
- Infections (79)
- Medication (109)
- Meditation (3)
- Mental Health (2)
- Neurology (6)
- OBGYN (33)
- Orthopedic (5)
- Patient Stories (85)
- Period Problems (17)
- Pregnancy (22)
- Psychiatry (6)
- Sexual Health (29)
- STDs (27)
- Urology (9)
Categories
- Allergy (12)
- Cancer (9)
- Cardiology (4)
- Dermatology (19)
- Endocrinology (1)
- ENT (25)
- format-2024 (9)
- Gastroenterology (20)
- Health Care (55)
- Infections (79)
- Medication (109)
- Meditation (3)
- Mental Health (2)
- Neurology (6)
- OBGYN (33)
- Orthopedic (5)
- Patient Stories (85)
- Period Problems (17)
- Pregnancy (22)
- Psychiatry (6)
- Sexual Health (29)
- STDs (27)
- Urology (9)
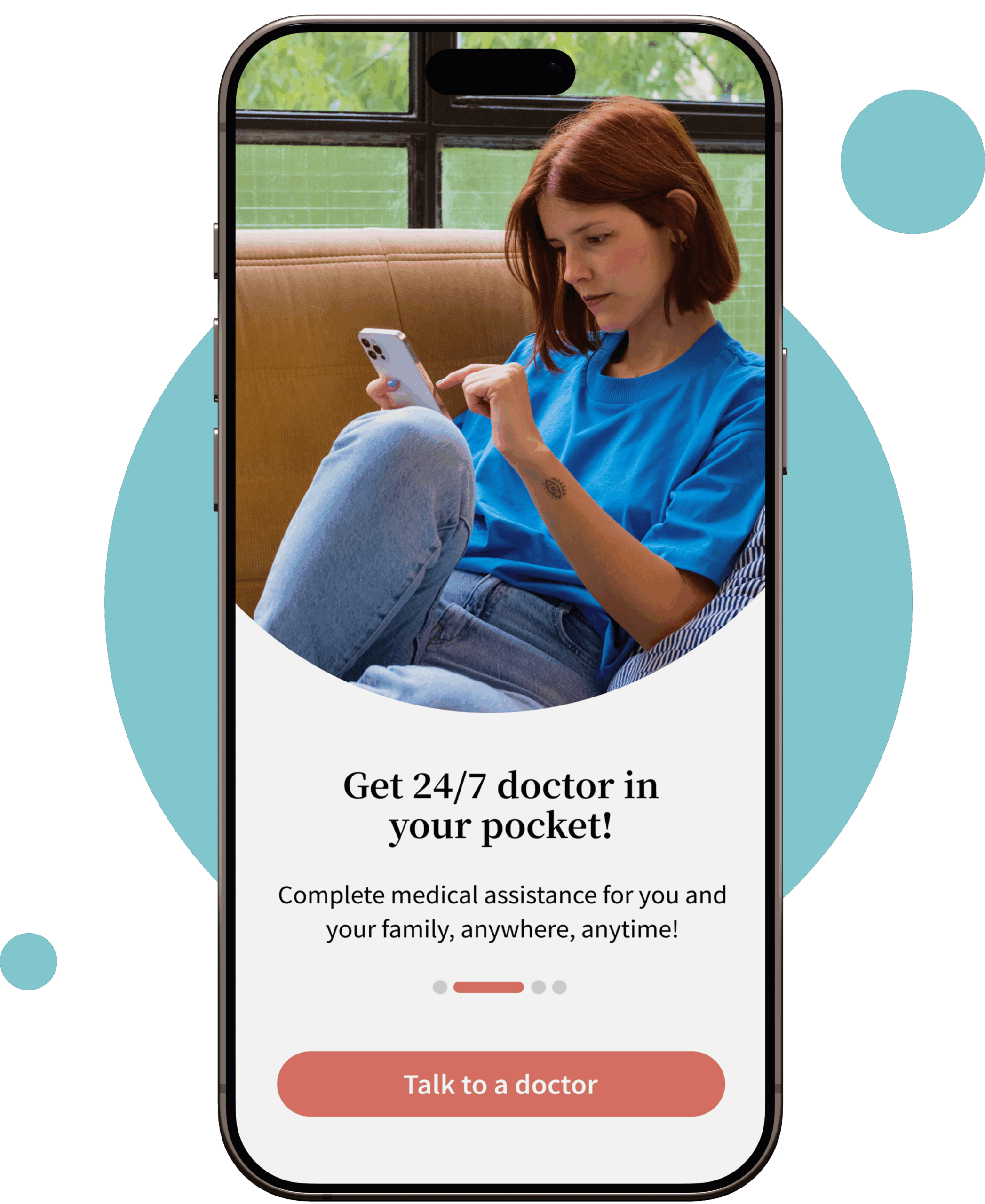
Get started today
Talk to online doctors now and get medical advice, online prescriptions, and referrals within minutes. On-demand healthcare services at your fingertips.