Table of Contents
ToggleOverview
Pneumonia is an inflammation of the lung tissues. It can involve a single or both lungs. The air sacs may fill with fluid (pus), causing cough with fever, phlegm, chills, and difficulty breathing. The causative organisms include:
- Bacteria
- viruses
- Fungi
Pneumonia can range from mild to life-threatening. It is most serious for:
- Infants
- Young children
- People older than age 65
- People having health problems or
- Weakened immune systems.
This article provides you with information on causes, risk factors, and how to diagnose and treat pneumonia.
What is Pneumonia?
Pneumonia is an inflammation of the lungs caused by acute infection and is characterized by recently developed signs of consolidation, both clinically and radiologically.
Types of Pneumonia
Pneumonia may be classified as:
1. Community-Acquired Pneumonia (CAP)
- This refers to an acute infection of the lung tissue acquired outside of the hospital. Community-acquired pneumonia (CAP) is a common disorder, with approximately 4–5 million cases diagnosed each year, 25% of which require hospitalization.
- It is the deadliest infectious disease and the eighth leading cause of death.
- Mortality is less than 1% in milder cases treated as outpatients.
- Among patients hospitalized for CAP, in-hospital mortality is approximately 10–12% and 1-year mortality (in those over age 65) is greater than 40%.
- Risk factors for the development of CAP include
- Alcoholism
- Advanced age
- Tobacco use
- Comorbid medical conditions, especially asthma or COPD
- Immune suppression
- Community-acquired pneumonia (CAP) is a leading cause of morbidity and mortality worldwide.
2. Nosocomial Pneumonia
- It is an infection of the lung tissue acquired in hospital settings and encompasses both hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP).
- Hospital-Acquired pneumonia (HAP)
- Ventilator-Associated pneumonia (VAP)
- These can be differentiated on the basis of settings, and infectious agents and require different diagnostic and therapeutic interventions.
- Anaerobic pneumonia and lung abscess can occur in both hospital and community settings and require separate consideration. It’s usually caused by a bacterial infection or a virus.
What are the Symptoms of Pneumonia?
Pneumonia symptoms may come on slowly over several days or they can develop suddenly over 24 to 48 hours.
1. Common Symptoms
- Cough
- It may be dry or produce thick yellow, green, brown, or blood-stained mucus (phlegm)
- Difficulty Breathing
- Breathing may be shallow, or rapid, and you may feel breathless while resting
- Tachycardia (Rapid heartbeat)
- Fever (High temperature)
- Feeling generally unwell
- Sweating and shivering
- Loss of appetite
- Breathing may be shallow, or rapid, and you may feel breathless while resting
- Chest Pain
- Gets worse when breathing or coughing
2. Less Common Symptoms
- Coughing up blood (hemoptysis)
- Headaches
- Fatigue
- Feeling sick or being sick
- Wheezing
- Joint and muscle pain
- Feeling disoriented and confused, particularly in elderly people
3. Symptoms in Young Children
Babies, especially newborns, may not show any symptoms, or their symptoms may be different from adults, including:
- Loss of appetite
- Vomiting
- Lack of energy
- Restlessness or fussiness
- Difficulty breathing or rapid breathing
- Fever, chills, general discomfort, sweating/ flushed skin
- Cough
Symptoms you can look for in babies and young children include:
- Limpness
- Crying more than usual
- Difficulty feeding
- Grunting sound with breathing or noisy breathing
- A decreased amount of pee
- Diapers that are less wet
- Pale skin
4. Symptoms in Adults (over 65 Years)
The elderly may experience :
- Cough
- Shortness of breath
- Symptoms of ongoing health conditions may worsen
- A sudden change in mental state
- Low appetite
- Fatigue
What’s the difference between viral and bacterial pneumonia?
1. Viral Pneumonia.
- Viruses are the most common cause of childhood pneumonia.
- In healthy young and middle-aged adults, viral pneumonia decreases in frequency, but it then increases substantially.
- During the past decade, the reported incidence of viral pneumonia has increased. Viral pneumonia can vary from a mild, self-limited illness to a life-threatening disease (depending on the virulence of the organism, as well as the age of the patient). Sometimes symptom management and rest are all that is needed for viral pneumonia. If it is severe your doctor may prescribe you an antiviral medication.
2. Bacterial Pneumonia
- It is an infection of your lungs caused by certain bacteria. The most common one is Streptococcus, but other bacteria can cause it too.
- These bacteria can live in your throat without causing any trouble if you are young.
- The most consistent presenting symptom of bacterial pneumonia is cough production of sputum.
- Antibiotic treatment is the most important component of drug therapy for bacterial pneumonia.
How Do You Get Pneumonia?
1. Pneumonia is Mostly Spread by
- Cough
- Sneeze
- Talk
- Sending respiratory droplets into the air which can then be inhaled by close contacts.
2. Pneumonia is Less Often Spread by
- Touching an object that has the germ on it and then touching your nose or mouth
What Causes Pneumonia?
Many germs can cause pneumonia. The most common pathogens are:
- Bacteria
- Virus
Your body usually prevents the above-mentioned germs from infecting your lungs. But sometimes these germs can beat down your immune system, even if your health is good.
These pathogens can spread via
- Coughing
- Sneezing
- Contaminating surfaces that people touch.
In most cases, a person contracts pneumonia-causing pathogens by breathing them into the small air sacs, or alveoli, within their lungs. The immune system acts by sending white blood cells to attack the infection, which sparks inflammation of the alveoli. The alveoli fill with fluid and pus and cause pneumonia.
How is Pneumonia Diagnosed?
Doctors will do an exam. They’ll check the person’s breathing pattern, appearance, and vital signs. Also, they’ll listen to the lungs and might suggest an X-ray.
The doctor may further ask you:
- If you are feeling breathless or breathing faster than usual?
- How long you have had a cough and whether you’re coughing up mucus?
- About the color of mucous?
- Is the pain in your chest worse when you breathe in or out?
- Measure your body temperature and listen to your chest and back with a stethoscope to check for any crackling or rattling sounds.
- The doctor may also listen to your chest by tapping it.
You probably will not need to have a chest X-ray or any other tests if you have mild pneumonia, but if your symptoms have not improved within 48 hours of starting treatment, then you may need a chest X-ray or other tests, such as a sputum (mucus) test or blood tests.
How Long Does Pneumonia Last?
Pneumonia is a serious illness that can take from a week to several months to fully recover, depending upon:
- How old are you?
- The severity of your illness
- Whether you have other health conditions
- What type of pneumonia do you have?
- How you care for yourself during this time
The path to recovery from pneumonia is as:
- Your chest may begin to feel better within four weeks
- Your cough and breathing may improve at six weeks
- You may feel a bit tired and finally symptoms free Within three to six months
1. In the Case of Mild Pneumonia
- After starting treatment your symptoms will begin to improve in one to two days
- Most people are able to return to their everyday activities in a week
- Fatigue and cough can linger for an entire month
2. In the Case of Severe Pneumonia
- Recovery timelines become foggier
- The majority of people continue to feel tired for about a month
It is better to talk with your doctor about when you can return to your normal activities.
Example of a Timeline for Recovery from Pneumonia
| Duration | Health Condition |
| Within seven days | Your temperature returns to normal |
| One month | Less mucus and your chest will feel better |
| Six weeks | Easier to breathe, and your cough is resolving |
| Three months | Tiredness and most of the other symptoms will be gone at this point |
| Six months | You should be back to normal |
How do you treat pneumonia?
1. Mild Pneumonia
- Can be treated at home with rest
- Use of antibiotics (if caused by a bacterial infection)
- Follow the Full Course of Antibiotic Treatment
- Most people start to feel better within two days after starting antibiotics, but it is important to continue taking your antibiotic treatment until the prescription is complete, otherwise, the bacterial infection and your pneumonia may come back.
- Painkillers, such as paracetamol or ibuprofen (do not take it if you are allergic to aspirin), may help relieve pain and reduce fever
- Drink plenty of fluids to avoid dehydration
- Gargling salt water
- Running a humidifier
2. Severe Pneumonia
- Treatment at a hospital might be necessary, especially for elderly ones
- You can get antibiotics and fluids through an intravenous (IV) line inserted into your vein
- You may also get oxygen therapy to increase the amount of oxygen in your blood
- If patients have severe symptoms and signs of pneumonia, breathing assistance through a ventilator in an ICU may be required
Is Pneumonia Contagious?
Whether it is bacterial or viral, both types of pneumonia are contagious.
Fungal and aspiration pneumonia are not contagious.
Complications
Complications are more common in young children, the elderly, and those with pre-existing health conditions, such as diabetes.
1. Possible Complications
- Severe Inflammation
- The thin linings between your lungs and ribcage become inflamed, which can lead to respiratory failure
- A Lung Abscess
- Mostly occur in people with a serious pre-existing illness or a history of severe alcohol misuse
- Sepsis
- Blood Poisoning
2. Potential Complications include
- An infection of the space that is in between the membranes which surround the lungs and chest cavity
- Inflammation of the sac surrounding the heart
- A blockage of the airway which allows air into the lungs
- A complete or maybe partial collapse of an entire lung or a specific area within the lung
You’ll be admitted to the hospital for treatment if you develop one of these complications.
Risk factors
Your body is designed to filter germs out of the air as you breathe. From nasal passages to the lungs. Nature has devised different mechanisms to prevent the body from acquiring diseases. Some conditions that change these mechanisms put the body at risk of developing infections.
Some of such risk factors that might weaken the body’s defenses and cause more severe forms even lethal complications of pneumonia are mentioned below :
1. Extremes of age
Being at extremes of age puts you at risk of developing pneumonia because the immune systems are weak in these populations. Their bodies have to work harder to fight infections
- Children 2 years old or younger
Infants and neonates have different physiological and anatomical respiratory characteristics compared to adults. The nasal passages are narrow so there is usually more mouth breathing. They are more prone to nasopharyngeal infections due to thin nasal mucosa and poor ability to disinfect the mucus. Their respiratory passages are also narrow. All these can lead to severe complications if the pneumonia is not diagnosed on time and treated appropriately. These complications include respiratory failure, meningitis, septicemia, and effusions
- People who are age 65 or older
Seniors have lean body mass, and comorbidities eg. Diabetes, vascular diseases, and cardiac diseases which increase the chances of complications. The complications may include, sepsis, pleurisy, ARDS ( Acute respiratory distress syndrome), and lung abscess.
Other risk factors include:
2. Lung Cancer
Lung cancer is a risk factor for pneumonia. Getting chemotherapy treatment for lung cancer might also increase a person’s pneumonia risk by reducing immune activity.
3. Being hospitalized
You are at greater risk of pneumonia if you are in an ICU, especially if you’re on a ventilator. Hospitalized patients are usually extremely sick with fragile immune systems. They have difficulty fighting off infections putting them at risk of developing pneumonia. Moreover, the germs present in hospital settings are usually stronger, more dangerous, and more resistant to medications as compared to those present in the community. This leads to more serious complicated pneumonia.
4. Chronic disease
You’re more likely to get pneumonia if you have asthma, chronic obstructive pulmonary disease (COPD), heart disease, or diabetes. These chronic diseases weaken the body’s immune system.
5. Smoking
You are not able to easily clear away mucus from respiratory passages. It damages your body’s defenses against the bacteria and viruses that cause pneumonia.
6. Weakened Immune System
People who have had an organ transplant, receive chemotherapy, long-term steroids, or HIV/AIDS.
7. Exposure to chemicals
Chemicals like radon, asbestos, and uranium. These damage the surface lining of the respiratory passages and make you prone to develop infections.
8. Air Pollution
Exposure to Air pollutants irritates respiratory passages and leads to lung cancers which increase the risk of developing pneumonia. They also cause chronic conditions like asthma and bronchiolitis which in turn are individual risk factors.
9. Drug and Alcohol Abuse
It can increase the risk of a specific type known as aspiration pneumonia. You are more likely to accidentally aspirate saliva or liquids in your respiratory passages in the unconscious or sedated state.
How to Prevent Pneumonia?
The best way to prevent it is to get a pneumonia vaccine against the bacteria and viruses that commonly cause it. Like flu shots, these vaccines won’t protect against all types of pneumonia, but if you do get sick, it’s less likely to be severe.
There are also everyday precautions you can take that may help reduce your risk of pneumonia.
- Good Hygiene
- Washing your hands regularly or using an alcohol-based hand sanitizer will protect you against respiratory infections
- Don’t Smoke
- Smoking destruct your lungs’ natural defenses against respiratory infections
- Good and Healthy Immune System
- Do exercise regularly, eat a healthy diet and get enough sleep
Stages of Covid Pneumonia?
COVID and pneumonia can be interlinked and occur simultaneously as a complication of COVID. It can even result in bilateral pneumonia or multifocal pneumonia.
Two stages of infection in patients with COVID-19 pneumonia are:
1. Early Phase
- There are high levels of the virus found in the lungs that trigger patients’ cells to express genes involved with the interferon pathway which is a critical part of the immune response.
2. Later Phase
- In this stage, the virus is no longer present, but the damage to the lungs is too severe for recovery.
The virus, in most cases, replicates in the nasal passages and then drops into the lungs, where it can cause pneumonia and other complications.
How to Treat Covid Pneumonia?
If you test positive and are more likely to get very sick from COVID-19, treatments are available that can reduce your chances of being hospitalized or dying from the disease.
Medications to treat COVID-19 must be prescribed by your doctor. The FDA has authorized certain antiviral medications and monoclonal antibodies to treat mild to moderate COVID-19 in people who are more likely to get very sick.
- Antiviral Treatments
- Target specific parts of the virus to stop it from multiplying in the body, helping to prevent severe illness and death.
- Monoclonal Antibodies
- Help the immune system recognize and respond more effectively to the virus.
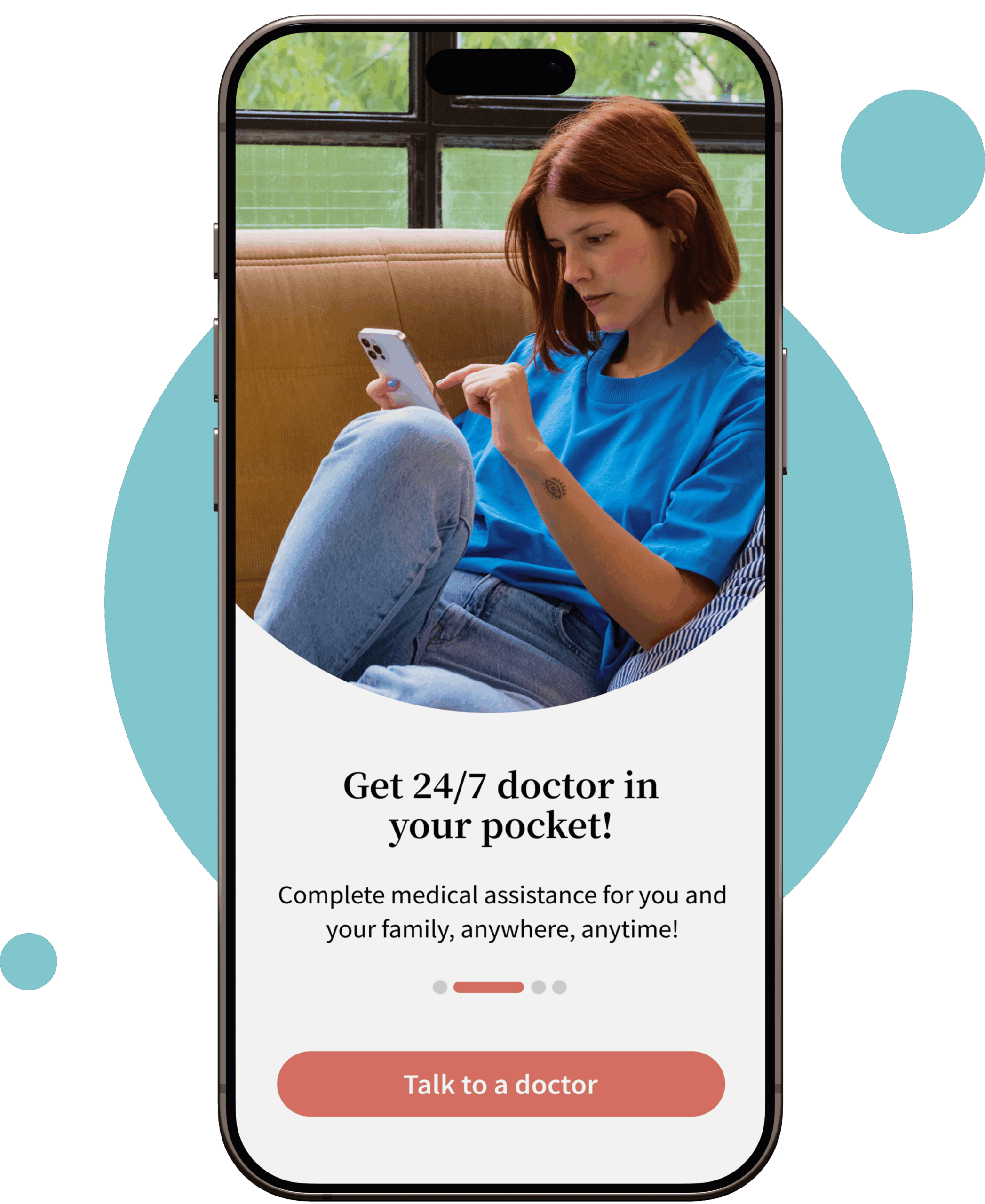
If you are COVID-positive and think you have developed pneumonia, consult our doctors for treatment options.
Is Pneumonia Contagious After Antibiotics?
Bacterial and viral forms of pneumonia are contagious. Whereas, chemical pneumonitis, fungal pneumonia (which mainly affects people with compromised immune systems), and aspiration pneumonia (caused by inhaling food or liquid into the airways) are not contagious.
- The time frame for Bacterial Pneumonia
- After starting antibiotics you are contagious for around 48 hours and your fever has gone away
- The time frame for Viral Pneumonia
- As symptoms start to go away, especially fever, so does the contagious period
When Should I See a Doctor?
If you have the following issues, now is the time to consult your doctor:
- Difficulty breathing
- Chest pain
- Persistent fever of 102 F (39 C) or higher
- Persistent cough, especially if you’re coughing up pus
Moreover, people in these high-risk groups should also see a doctor:
- Adults older than age 65
- Children younger than age 2 with signs and symptoms
- People with a weakened immune system or underlying health condition
- People taking medication that suppresses the immune system or receiving chemotherapy
Note: For older adults and people with heart failure or chronic lung problems, pneumonia can quickly become a life-threatening condition.
FAQs About Pneumonia Answered By your Doctor Online Team
COVID and pneumonia can be interlinked and occur simultaneously as a complication of COVID. It can even result in bilateral pneumonia or multifocal pneumonia.
Symptoms of COVID-19 can appear from 2 to 14 days after you’ve been exposed to the virus.
Mild Disease
Recovery Time: About 2 weeks
Symptoms: Upper respiratory tract infection, fever, cold and cough, and other mild symptoms such as headache or conjunctivitis
Moderate to Severe Disease
Recovery Time: 3-6 weeks
Symptoms: A severe disease can cause pneumonia. 50% of people have low oxygen levels due to shortness of breath. Most patients will have a fever, feel very tired, and have a dry cough.
Critical Disease
Recovery Time: Varies by person
Symptoms: Severe COVID-19 and pneumonia can lead to critical illness, including acute respiratory distress syndrome (ARDS), cardiac disease, organ dysfunction, and shock.
If you are recovering from COVID pneumonia and experiencing persistent problems, I recommend seeing your doctor for a follow-up evaluation.
Some of the tips are:
1. Get plenty of rest and sleep
2. Slowly start moving around once you’re ready
3. Complete all treatments prescribed by your doctor
4. Good nutrition helps your body recover
5. Stop smoking. Breathing in smoke can worsen your condition
6. Limit exposure to throat irritants, including pollution and alcohol
7. Perform deep breathing exercises
8. Get plenty of water to stay hydrated
9. Consult with your doctor before returning to exercise
Pneumonia is informally described as walking pneumonia if the patient has a milder form of symptoms and does not require hospitalization or bed rest.