Allergy treatment & prescriptions online
Particularly prevalent during springtime, allergies often disrupt daily life and can lead to frequent sick leave. At Your Doctors Online, we understand the impact allergies can have on your well-being. That’s why we offer convenient access to specialized allergy doctors through our online platform. Say goodbye to long waiting times and cumbersome appointments; with just a few clicks, you can connect with an experienced doctor for personalized treatment.
Don’t let allergies dictate your life. Take control of your health today by seeking relief from allergy symptoms with the help of our dedicated team of professionals at Your Doctors Online.
How to connect with an allergy doctor?
Connect with allergy doctor online in 3 easy steps.
1
Describe your issue
Download our app, register and tell us about your medical issue to get started.
- Cold/Flu
- STD
- UTI
- Sexual Health
- Skin
- Allergies
2
Chat with a doctor
Connect with a board-certified doctor. You can chat, send pictures and videos.
3
Get a prescription
Our online doctors can help you with your medical issues and give you prescriptions.
Prescription
- Loratadine 10mg one tablet daily
- Use for 5 days
Send Prescription
Identifying allergy symptoms
Do you find yourself experiencing any of the following seasonal allergy symptoms?
- Sneezing
- Watery or red eyes
- Cough
- Red rashes
- Swollen eyes or face
- Vomiting
If so, you’re not alone. Many individuals struggle with these discomforts, often seeking relief from the burdensome effects of allergies. Recognizing these symptoms is the first step towards finding effective treatment. At Your Doctors Online, we’re here to help you navigate through your allergy symptoms.

Causes of allergies
Allergies occur in various forms, each with its own set of triggers:
- Seasonal allergies (Allergic rhinitis or hay fever): These allergies are often prompted by plant pollen, prevalent during specific seasons.
- Allergic asthma: Triggered by allergens such as dust mites, this condition can lead to asthmatic symptoms.
- Food allergies: Certain foods, like shellfish, peanuts, soy, milk, and wheat, can prompt allergic reactions upon ingestion.
- Drug allergies: Reactions to specific medications, such as certain antibiotics, can manifest as drug allergies.
- Latex allergies: Allergic reactions to latex materials, like rubber gloves, fall under this category.
How to treat allergies?
For more severe allergies or symptoms that are not adequately controlled with OTC medications, prescription options may be necessary. These can include nasal steroid sprays and stronger antihistamines, which your doctor can prescribe based on your specific needs. Examples include:
- Feofenadine
- Levocetirizine (Xyzal)
- Loratadine (Claritin)
Remember, if you suspect you are experiencing anaphylaxis, do not hesitate to use your epinephrine auto-injector and seek immediate medical attention. Allergies can vary in severity, so it’s essential to work closely with your healthcare provider to develop an effective treatment plan tailored to your individual needs.
FAQs about allergies treatment
When should I see an allergist or immunologist?
Consider consulting an allergist if you experience symptoms such as chronic sinus infections, nasal congestion, or difficulty breathing due to allergies. Additionally, persistent hay fever or year-round allergy symptoms warrant a visit to an allergist for proper evaluation and management.
What is the most effective allergy treatment?
For preventing symptoms, antihistamines and nasal steroids are often recommended, especially taken daily before allergy season begins. Intranasal steroids are currently regarded as the first-choice treatment for individuals with persistent allergy symptoms.
How can I permanently stop allergies?
Unfortunately, there's no permanent cure for allergies. However, symptom relief can be achieved through OTC or prescription medications. Avoiding allergy triggers and minimizing exposure to them can also help prevent allergic reactions. Immunotherapy may gradually reduce the severity of allergic reactions over time.
How long does it take for allergy medicine to work?
Antihistamines, used for allergy treatment, typically start working within 1 to 2 hours.
How long does an allergic reaction last?
Most allergic reactions take a few hours to settle down. With timely treatment, it can settle down within an hour. In case of a severe allergic reaction, you may need to visit your local A&E for medical assistance.
What is the best allergy medicine for pollen?
Most allergic reactions take a few hours to settle down. With timely treatment, it can settle down within an hour. In case of a severe allergic reaction, you may need to visit your local A&E for medical assistance.
How long does it take to get an allergy test?
An allergy blood test typically takes about 10 minutes, as it involves giving a blood sample. A skin prick test may take three to five minutes per allergen, plus a waiting period of 15 to 20 minutes to observe any reactions. Similarly, a patch test may also take three to five minutes per allergen. You can get a lab requisition for allergy test from our online doctor at Your Doctors Online.
What is the safest antihistamine to take long term?
Fexofenadine (Allegra) is considered one of the safest long-term options among second-generation antihistamines. It is less sedating compared to other options and generally well-tolerated. However, as with any medication, rare side effects may occur, so it's important to follow your doctor's guidance.
Which antihistamine is best for severe allergies?
Some commonly recommended antihistamines for severe allergies include: Benadryl (diphenhydramine) Claritin (loratadine) Allegra (fexofenadine) Zyrtec (cetirizine) Xyzal (levocetirizine)
What are common allergy triggers?
The following are some of the common allergy triggers:
· Airborne triggers like pollen, dust, insect dander, mold etc
· Specific foods which may include peanuts, soy, fish, wheat, milk, etc
· Bee or wasp stings
· Some medications like penicillin
Related Blog Articles

Can allergies make you cough?
Overview If you’ve ever asked yourself, “Can allergies make you cough?” you’re not alone. Many

Am I sick, or is it allergies?
Overview As the saying goes, “Know thy enemy.” When it comes to distinguishing between a

Can allergies cause sore throat, how to treat it?
Overview One of the most bothersome allergy symptoms that can disrupt daily life is a
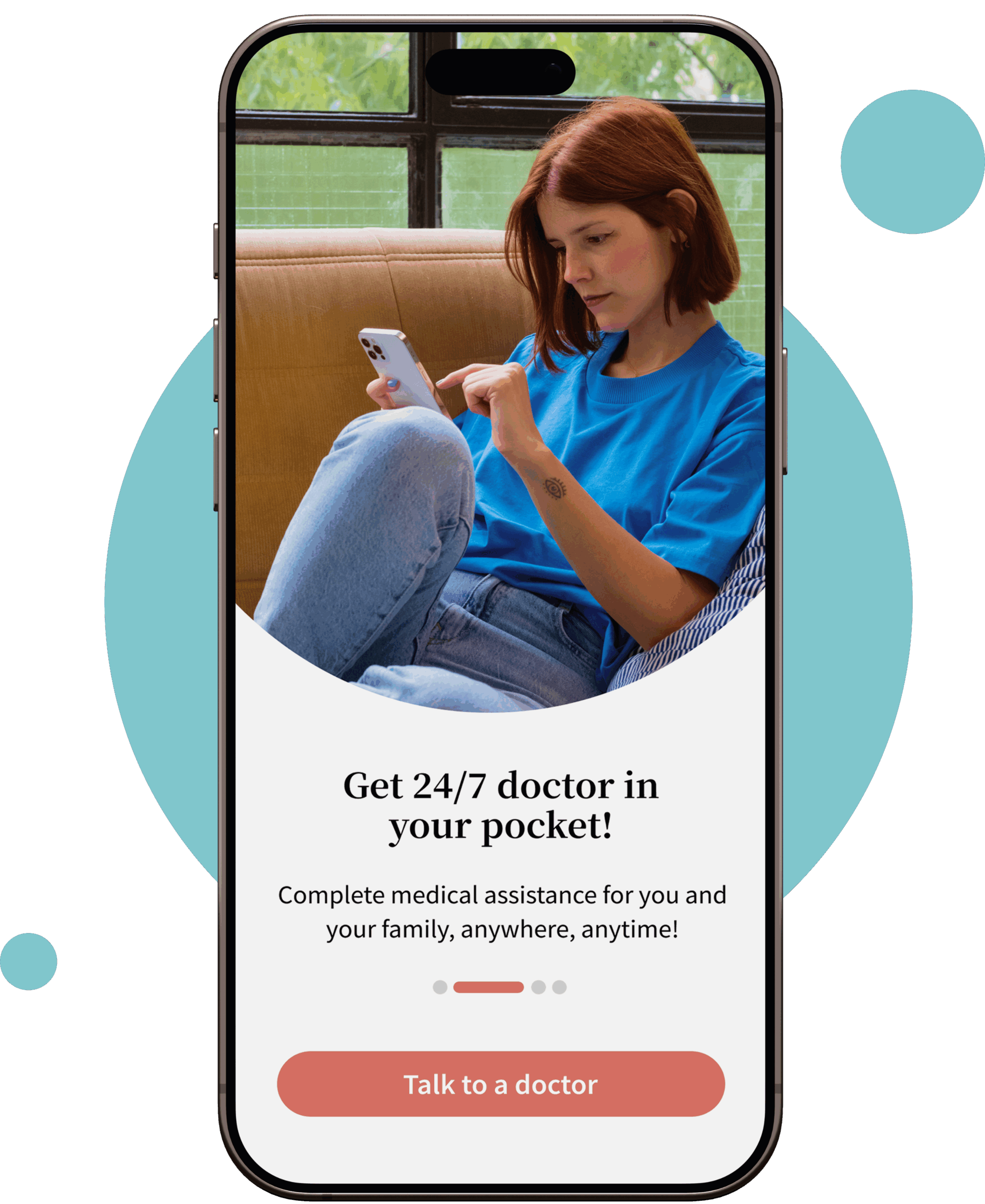
Get Started Today
Talk to online doctors now and get medical advice, online prescriptions, refills, lab requisitions and medical notes within minutes. On-demand healthcare services at your fingertips.