Many women only discover they have polycystic ovary syndrome (PCOS) when they start trying to get pregnant. Their symptoms were ignored, dismissed, or misdiagnosed for years.
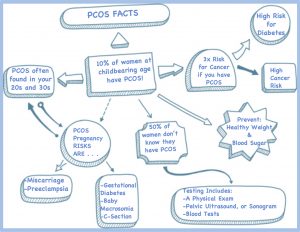
While it’s commonly said that about 10% of women have PCOS, some research suggests the real number may be much higher, possibly close to one in four. That makes PCOS one of the most common causes of infertility in women.
The good news: PCOS does not mean you can’t get pregnant. But it does mean you may need support, planning, and sometimes treatment to ovulate regularly and carry a healthy pregnancy. You can start by seeing an online doctor for pregnancy consultation.
What is Polycystic Ovarian Syndrome?
Polycystic ovary syndrome is the most common endocrine (hormone) disorder in women of reproductive age. It can start as early as age 11 and continue until menopause.
Hormonal Imbalance
In PCOS, the ovaries make higher-than-normal levels of androgens (male hormones).
Women naturally have both estrogen/progesterone (female hormones) and small amounts of androgens. In PCOS:
-
Androgens are too high
-
Estrogen and progesterone balance is disrupted
-
Ovulation becomes irregular or stops
Because these hormones control your menstrual cycle, the imbalance interferes with egg development and release, which is why PCOS is so strongly linked to infertility.
How PCOS Affects Your Ovaries
Normally, each month:
-
Several follicles (fluid-filled sacs) form in the ovary
-
One follicle matures and releases an egg (ovulation)
-
The egg can then be fertilized and implant in the uterus
In PCOS:
-
The ovaries make too many androgens
-
Multiple follicles form, but don’t mature properly
-
Eggs stay “stuck” and are never released
-
Ovulation becomes sporadic or absent
That’s where the term “polycystic” comes from. They are not true cysts, but many immature follicles that never release eggs.
Without regular ovulation, your levels of:
-
Estrogen
-
Progesterone
-
Follicle-stimulating hormone (FSH)
-
Luteinizing hormone (LH)
also shift. This leads to irregular periods, trouble tracking fertile days, and difficulty conceiving.
How do I know if I have PCOS?
Only a doctor can diagnose PCOS, but tracking your symptoms can help you know when to seek help.
Common symptoms of PCOS
You may notice:
-
Persistent adult acne: Acne that doesn’t respond well to usual treatments, especially along the jawline, chin, or back.
-
Excess facial or body hair (hirsutism): Hair growth on the face, chest, stomach, or back. About 70% of women with PCOS have hirsutism.
-
Hair thinning or hair loss on the scalp: Shedding on your pillow, in the shower, or widening at the part line.
-
Weight gain or trouble losing weight: Individuals with hormone imbalances may also experience difficulties maintaining a healthy weight. This is because obesity is closely tied to PCOS. The hormones in your body play a role in determining your appetite and metabolism. Between 40 and 80% of women who suffer from PCOS were reported to be overweight or obese.
-
Type 2 diabetes or insulin resistance: Up to 70% of women with PCOS have insulin resistance. This can raise blood sugar and increase the risk of diabetes.
-
Skin darkening and skin tags: Acanthosis nigricans (dark, velvety patches) in the neck, armpits, under the breasts, or groin. Small skin tags are also common and often linked to insulin resistance.
-
Irregular or absent periods: Fewer than 8 periods a year, very long cycles, or no period at all. That makes it hard to predict ovulation or fertile days.
-
Fertility problems: Difficulty getting pregnant after 6–12 months of trying may be the first sign for many women.
These symptoms can affect your self-esteem and emotional health. Even though there is no cure for PCOS, there are effective ways to manage symptoms and improve your chances of getting pregnant.
If you recognize multiple signs, it’s worth discussing PCOS with a doctor.
Can you get pregnant with PCOS?
Yes.
PCOS is a leading cause of infertility, but it does not mean pregnancy is impossible.
The main issue is irregular or absent ovulation, not that your body can never rerelease eggs. Many women with PCOS:
-
Conceive naturally with lifestyle changes
-
Conceive with the help of fertility medications
-
Conceive using assisted reproductive techniques like IUI or IVF
The goal is straightforward: to help you ovulate more regularly and at the optimal time.
Natural approaches and lifestyle changes
Lifestyle changes are often the first step in PCOS fertility treatment, especially if you are overweight or insulin-resistant.
Weight loss and ovulation
Studies show that losing 5–10% of your body weight can:
-
Improve insulin sensitivity
-
Help regulate hormones
-
Restart or improve ovulation
-
Increase the chance of conception
Even modest weight loss can make a difference. Helpful strategies include:
-
Whole-food, balanced meals (lean protein, fiber, healthy fats)
-
Reducing refined carbs and sugar
-
Regular physical activity
-
Managing stress and sleep
These changes support both fertility and long-term health.
Fertility medications for PCOS
Many women with PCOS need medication in addition to lifestyle changes to trigger ovulation.
1. Clomiphene (Clomid)
-
One of the most commonly prescribed fertility drugs for PCOS
-
Taken orally for a few days early in the cycle
-
Works by stimulating the brain to release more FSH and LH, which encourage ovulation
Your doctor may start with Clomid and monitor ovulation with blood tests and ultrasounds.
2. Letrozole
-
Originally developed as a breast cancer medication
-
Now widely used off-label as an ovulation inducer in PCOS
-
Some studies suggest higher pregnancy rates than Clomid in women with PCOS
Letrozole is often used when Clomid has failed or as a first-line option, depending on your doctor’s approach.
3. Metformin
-
A medication used for type 2 diabetes and insulin resistance
-
Improves insulin sensitivity
-
Can help regulate cycles and support ovulation, especially when combined with other fertility drugs
-
Helpful if you have both PCOS and high insulin or blood sugar issues
Your doctor may combine Metformin with Clomid or Letrozole for better results.
Assisted fertility treatments: IUI, IVF, and IVM
If oral medications are not enough or other fertility factors are present (like male factor infertility), assisted reproductive techniques may be recommended.
Intrauterine insemination (IUI)
-
You may take fertility drugs to stimulate egg growth
-
Your partner’s (or donor’s) sperm is washed and placed directly into the uterus with a thin catheter
-
Timed around ovulation to increase chances of fertilization
In vitro fertilization (IVF)
-
Fertility drugs stimulate the ovaries to produce multiple mature eggs
-
Eggs are retrieved from your ovaries before ovulation
-
Eggs are fertilized with sperm in the lab
-
One or more embryos are then transferred into the uterus
IVF allows very close control of egg development, fertilization, and embryo selection.
In vitro maturation (IVM)
-
A newer option some women with PCOS may consider
-
Immature eggs are retrieved without high-dose stimulation
-
Eggs mature in the lab
-
Once mature, they are fertilized and transferred as in IVF
IVM may reduce the risk of overstimulation, which can be a concern in PCOS.
Is there a cure for PCOS?
No. There is currently no cure for PCOS. However, the symptoms are highly manageable, and fertility can often be significantly improved with:
-
Lifestyle changes
-
Medications
-
Fertility treatments when needed
Even if you are not trying to conceive, treating PCOS is important to reduce long-term health risks.
PCOS pregnancy risks
Women with PCOS have a higher risk of certain complications during pregnancy, including:
-
Miscarriage
-
Preeclampsia
-
Gestational diabetes
-
Cesarean section (C-section)
-
Macrosomia (larger babies, over about 8 lb 13 oz)
You can lower your risk by:
-
Reaching a healthy weight before pregnancy, if possible
-
Optimizing blood sugar and insulin levels before conception
-
Taking folic acid as recommended by your doctor
-
Getting early and regular prenatal care
Your doctor can create a pregnancy plan tailored to your risks and health history.
Other long-term health risks of PCOS
PCOS is more than a fertility issue. It can increase your risk of:
-
Type 2 diabetes
-
High blood pressure
-
High cholesterol
-
Sleep apnea
-
Depression and anxiety
Some studies also suggest links with breast and ovarian cancer. These risks are another reason why diagnosis and long-term follow-up matter, even if pregnancy is not your current goal.
How is PCOS diagnosed?
Your doctor may use:
-
Medical history and symptom review
-
Physical exam (including weight, blood pressure, hair growth, skin changes)
-
Pelvic ultrasound to assess the ovaries and uterine lining
-
Blood tests to check hormone levels, blood sugar, and cholesterol
Because PCOS can mimic other conditions like thyroid disease or high prolactin, your doctor will rule out other causes before confirming a diagnosis.
When should I see a doctor?
Talk to a doctor if:
-
Your periods are very irregular or absent
-
You’ve been trying to conceive for 6–12 months without success
-
You have persistent acne, excess hair, or hair loss
-
You have signs of insulin resistance (dark skin patches, weight gain, cravings)
-
You’re worried about PCOS or fertility in general
Early diagnosis allows you to:
-
Protect your future fertility
-
Lower your risk of diabetes and heart disease
-
Get support managing weight, mood, and hormones
-
Plan a safe, healthy pregnancy when you’re ready
Get answers to your PCOS and fertility questions
You don’t have to guess what’s going on with your cycles, hormones, or fertility. If you’re worried about PCOS, struggling to get pregnant, or recognizing the symptoms above, a doctor can help:
-
Review your symptoms and provide PCOS treatment online
-
Provide lab test requisitions for PCOS (pelvic ultrasound, sonogram, blood tests)
-
Discuss options like lifestyle changes, fertility meds, IUI, or IVF
Consulting a doctor is the fastest way to determine your current health status and identify your next steps.




